Medics have not always linked raised intraocular pressure with the apparition loss from glaucoma. Though several persons appear to have observed firmness of the eye in this disorder as far back as the 10th century, raised intraocular pressure was not regularly measured until the latter part of the 19th century. von Graefe industrialized the first tool for gauging intraocular pressure in 1865. The first sensibly precise tool was the Malakoff applanation tonometer of the late 19th century; it was in extensive use throughout Eastern Europe until comparatively lately. Schiötz industrialized an indentation tonometer that was extensively used throughout the world throughout the first two-thirds of the 20th century. Goldmann’s applanation tonometer of 1950 commenced the epoch of truly precise intraocular pressure extent. It is still the most extensively used tonometer in the ecosphere.
Other expedients such as the McKay-Marg tonometer (or its descendants the Tono-Pen), the pneumatonometer, and air-puff applanation tonometers are expanding supporters. The active outline tonometer is the first completely new notion in tonometry in over 100 years. It is perhaps the most precise of all the tonometers that one can purchase from healthcare industry suppliers and is comparatively autonomous of corneal biomechanical possessions distinct from its precursors. Transpalpebral tonometers are striking as they do not need current anesthesia; though, they add the biomechanical possessions of the eyelid to the tilt of possible mistakes and have not been demonstrated very precisely. The future must, with any luck, bring tonometers that can give daytime or even lengthier signs of intraocular pressure difference. Though intraocular pressure promotion (or its absenteeism) no lengthier can be totaled for analytic drives, the part of intraocular pressure in the administration of glaucomatous optic neuropathy remains significant.
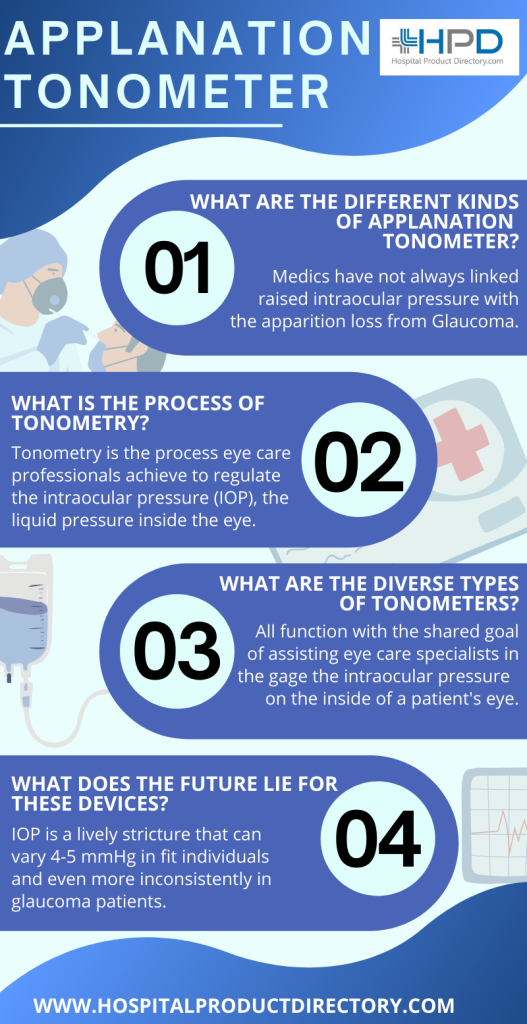
What is the process of Tonometry?
Tonometry is the process eye care professionals achieve to regulate the intraocular pressure (IOP), the liquid pressure inside the eye. It is an imperative examination in the assessment of patients in danger from glaucoma. Most tonometers are standardized to gauge pressure in millimeters of mercury (mmHg).
What is Glaucoma?
Glaucoma is the foremost cause of sightlessness in persons over the age of 60 and is produced by an augmented sum of liquid pressure inside the patient’s eye. This augmented burden can damage the patient’s optic nerve. Since glaucoma can ultimately reason blindness if it goes untouched, a tonometry examination is a vital share of the investigation for noticing variations in the eye as early as conceivable. The definite kind of tonometer used will be contingent on the patient and the doctor’s penchant.
What are the diverse types of tonometers?
Although there are numerous diverse kinds of tonometers available with Applanation Tonometer suppliers, they all function with the shared goal of assisting eye care specialists in the gage the intraocular pressure (IOP) on the inside of a patient’s eye. The IOP extent aids optometrists and ophthalmologists regulate a patient’s danger of developing glaucoma.
Digital Contact Tonometers
The Digital Applanation Tonometer (D-KAT) is a numeral form of the KAT applanation tonometer. The Digital Applanation Tonometer functions are founded on the ‘Goldmann technique,’ which entails it computes IOP from the force obligatory to compress a steady part of the patient’s cornea. This expedient bid user excellent dependability and ease of use. It aspects a LED display and inner microchip technology that permits for the precise and immediate depth of IOP. To further abridge the process, the D-KAT has an illumined display that eases easy interpretations, even in the dimmest of inspection quarters. The D-Kat is obtainable in both Take-away as well as Immovable alternatives and is well-matched with most slit lamps.
Standard Contact Tonometer
The standard contact tonometer is founded on the Goldmann applanation tonometry (GAT), which is the most shared and documented as the international gold normal for gauging IOP. This technique includes consuming a tonometer tip to trace an asleep cornea to determine the quantity of force obligatory to compress the cornea. Throughout this process, the eye care expert will turn the tension handle varying the corneal force. The IOP will be regulated when the inner facets of the two semicircles get in touch with each other.
Perkins Hand-Held Tonometer
Alike to the standard contact tonometer, the Perkins tonometer uses the same applanation prisms. Though, the Perkins tonometer is moveable and can be consumed for patients who:
- Are being tried in the prostrate location
- Have corporal boundaries that stop them from placing in a slit lamp
- Aren’t being verified in the workplace with a slit lamp
Non-Contact Tonometer (NCT)
A non-contact tonometer or a pneumotonometer includes smearing a quick wisp of air pressure to the patient’s eye through an apparatus. The quick wisp of air compresses the patient’s cornea in a non-invasive way, which entails the eyes do not have to be anesthetized before the examination. The force obligatory to compress the patient’s eye is noticed by radars to regulate the patient’s IOP. In the occurrence of the patient has irregular consequences, the doctor should complete other examinations to approve the analysis. These gadgets have augmented incorrectness to the Goldmann applanation tonometry (GAT) and in most nations, you must prove correctness to Goldmann before getting promotion permission (FDA).
The Accutome AccuPen
The AccuPen is a handheld automated expedient that is molded like a large indicator. It uses a minute plunger to regulate the amount of defiance given by an asleep cornea when contacted. Gravity Equipoise Skill offers exact IOP capacities with less standardization likened to other handheld tonometers available with Applanation Tonometer dealers. Micro strain device technology shared with branded systems delivers reproducible consequences.
The AccuPen can be effortlessly shipped and bids the most compensation when used on a patient’s edematous or damaged cornea. The Accu-Pen, though, necessitates a latex throwaway tip, which means it may not be a feasible answer for patients with latex aversions.
Rebound Tonometer
Rebound tonometry undertakes that patients with a complex IOP or those with more solid eyes will encourage an earlier deceleration of a probe than patients with a truncated IOP or laxer eye. A rebound tonometer actions the introduction current produced when the metallic probe recoils or ricochets off of the cornea back to the expedient. The speed of the ricochet is transformed into mm Hg. The technique of rebound tonometry doesn’t necessitate anesthesia and can gauge IOP relatively rapidly.
what does the future lie for these devices?
IOP is a lively stricture that can vary 4-5 mmHg in fit individuals and even more inconsistently in glaucoma patients. Developments have been made to mature methods that can screen IOP beyond the in-office dimensions. Early animal education has examined know-how for enduring IOP observing, counting the surgical embedding of a pressure transducer scheme, as well as the establishment of an intraocular device into the lens capsule.
The main disadvantages of these plans include the operating risks. The main expedient industrialized for temporary IOP observing is the soft contact lens sensor (CLS) that gauges variations in ocular scopes over a 24-hour period, which has exposed good association with true IOP in vitro manometry education. This expedient is presently accepted in Europe for medical use. The main disadvantages of this skill include trouble understanding the volume of amassed data, as well as the incapability of the yield signal to be unswervingly interpreted into clinically used mmHg gage To find the best tonometers in India, please log onto the Hospital Product directory as it is a web portal that meets the requirements of the Medical industry.
