Today, with innovative Gynecology, Andrology, and IVF treatments, numerous couples struggling with childlessness issues are grasping their dreams of becoming parents. Sterility can be female sterility or male infertility. The most shared reasons for female sterility are issues with ovulation, cervix problem, and damage to the fallopian tube or uterus. Semen quality or Varicocele are shared male sterility-related issues. Medical apparatus made by IVF Equipment Manufacturers are playing a significant role in vastly refining sterility treatments and better outcomes. In this blog, we will examine the various equipment that is required in an IVF center and an Andrology Center.
Equipment for IVF room
Intra-uterine impregnation (IUI) is a process for placing washed/ cleaned sperm in a uterus during the ovulation period. The objective of IUI is to surge the number of semen that reach the fallopian tubes and subsequently surge the chance of insemination. This process is valuable if semen count or motility is poor.
1. Sperm Counting chamber- For counting the number of semen and examining the motility of semen with high precision, efficiency, and ease. The Chamber guarantees uniform conditions for all of the examined samples; it confirms a more accurate assessment of motility as it allows free movement of sperm that are consistently dispersed in a friction-free single horizontal plane. The precision of examination is heightened through the removal of the various steps required by the usual hemocytometric method.
2. Laminar Airflow– The laminar flow machines are used to deliver a disease-free environment for the medical machines to uphold a clean environment. These are completed to meet spotless air as per the necessities with help of percolation, lighting, Noise, and Vibration. Laminar Flow Units are available with IVF Equipments Suppliers with Vertical airflow arrangement.
3. Centrifuge– This instrument has been devoted to refining the total motile semen recovery from the parent sperm sample, by controlling/upholding the main stricture of “Temperature” thus meant at Enhancing the ART outcomes. The instrument has been intended to regulate and then uphold the “Critical” inner chamber temperature before, after, and during centrifugation. The warming array of the Centrifuge’s cavity is from 2°C above ambient to 42°C. The gifted control system does not permit the centrifugation to begin till the set temperature is achieved. Though, one does have the option to begin the centrifugation without chamber heating and to begin the chamber heating without centrifugation.
4. Test tube warmer- It is extensively used for sterility and sperm analysis clinics or laboratories. It is Used to uphold the temperature of egg (oocyte) gathering tubes at or near body temperature. Intended to admit up to 6 Falcon® 2001 test tubes.
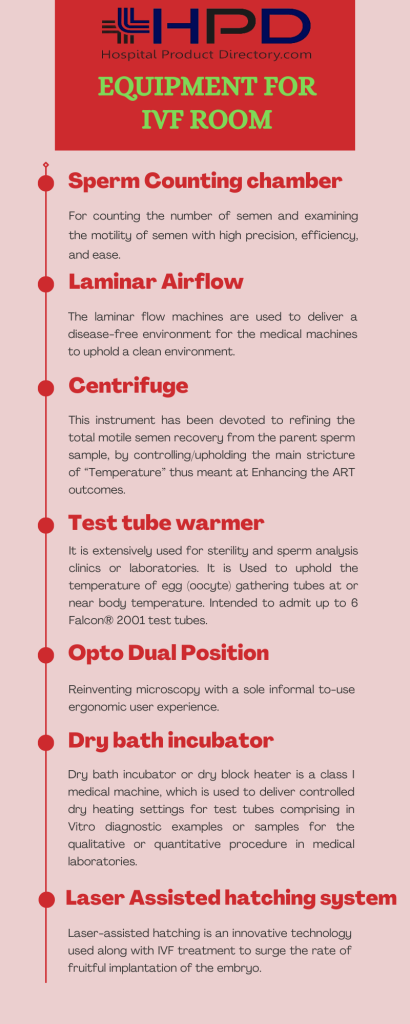
5. Opto Dual Position: Reinventing microscopy with a sole informal to-use ergonomic user experience. Ultra-high disparity macro and micro imaging from the same tool eradicates the need for 2 separate microscopes Intended for ‘in the chamber’ Biomed and cell examination applications such as IVF and other cell business applications – no more transporting samples between terminals! Embraces the new Opto ‘E-mirror’ LED lighting system with mutable intensity and color temperature to safeguard the best contrast for a high-quality picture.
6. Dry bath incubator– Dry bath incubator or dry block heater is a class I medical machine, which is used to deliver controlled dry heating settings for test tubes comprising in Vitro diagnostic examples or samples for the qualitative or quantitative procedure in medical laboratories. A dry block heater plays an energetic role in the incubation and initiation of cultures, enzyme responses, clotting studies, enzyme responses, inactivation of sera, and restraint digests.
7.Laser Assisted hatching system- Laser-assisted hatching is an innovative technology used along with IVF treatment to surge the rate of fruitful implantation of the embryo. Laser-assisted hatching is done just before the embryo transfer process and can be done on embryos at the early cleavage steps (that is two or three days after the egg gathering) and at the blastocyst phase (five or six days after the egg gathering).
8. The EmbryoScope permits infertility specialists to screen the progress of inseminated embryos around the clock without confiscating them from the protected incubator. This gives doctors and patients a vision of how the embryo is evolving. For many patients, it has enhanced their chances of realizing a pregnancy. Though the technology can be used for any kind of patient to advance their time to pregnancy, its assistance is best seen when we arrange the usually developing embryos over embryos that have done improper or irregular developmental processes during incubation. Without the use of the EmbryoScope, the embryologist is not able to recognize if an embryo has shadowed the normal path of expansion and has the highest chance to yield a pregnancy.
Equipment for Andrology Lab
Sperm Analyzer – A semen examination, also called a sperm count, gauges the quantity and quality of ejaculate and semen. Ejaculate is the dense, white liquid released from the penis during the sensual climax (orgasm). This issue is named ejaculation. Sperm contains semen, the cells made in the male generative system that comprise the genetic material required to make a baby. A semen examination is used to find out if a hindrance with ejaculation or sperm may be producing infertility.
Cell counters deliver additional recompences beyond time and labor savings and augmented accuracy, allowing cell biology researchers to conduct trials using previously unobtainable methods. Unlike a hemocytometer, an innovative automated cell counter such as Bio-Rad’s TC20™ cell counter features user-defined gating for cubicle size. This attribute permits discerning cell counting within a size range. This improvement permits the counting of subpopulations within mixed populations with manifold cell sizes. This is a treasured ability for procedures using coculture and for key cells inaccessible from tissue or organs. The aptitude to the gate for size meaningfully enlarges the utility of automated cell counters bought from IVF Equipments Dealers.
The andrology and semen examination microscope is used for inspecting both the quality and quantity of sperm. Andrologists use phase disparity when they do not want to tinge a sample to view the form of the semen. Sperm examination microscopes include a heated stage bowl and controller, which permits the sperm to remain living, which is vital in andrology examination.
